Postnatal Depression Survival Guide
A Postnatal Depression Survival Guide
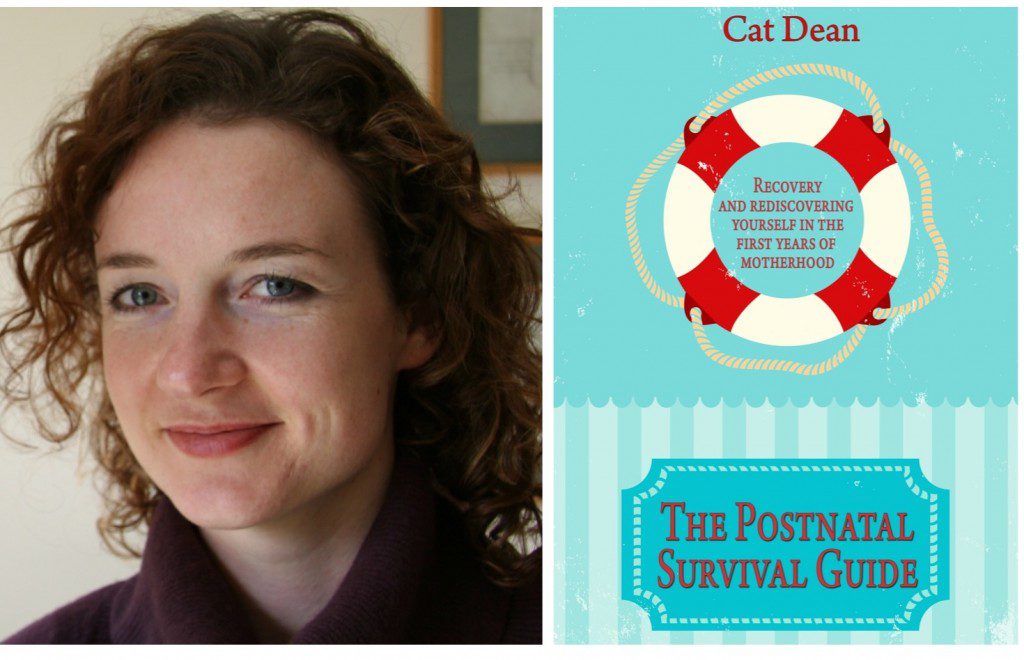
Today’s post is a guest post from the brilliant Cat Dean, who blogs at www.postnatalsurvival.com and is author of Fertile Thinking and The Postnatal Survival Guide. You can also read more from Cat over on TalkMum (my new work project – more on this later). Thanks Cat!
 I read a really interesting piece on the BBC website this week – professor of clinical psychology Dr Peter Kinderman argues that we should stop pathologising ‘normal’ human emotions such as grief and anxiety – and offer sufferers understanding and sympathy in place of medication.
I read a really interesting piece on the BBC website this week – professor of clinical psychology Dr Peter Kinderman argues that we should stop pathologising ‘normal’ human emotions such as grief and anxiety – and offer sufferers understanding and sympathy in place of medication.
The piece comes ahead of the publication of the American Psychiatric Association’s Diagnostic and Statistical Manual (DSM -5) – the handbook from which clinicians will diagnose and treat mental illnesses. Dr Kinderman is concerned that more and more behaviours such as grief following bereavement, or childhood temper tantrums, are being relabelled “major depressive disorder” and “disruptive mood dysregulation disorder” respectively. As soon as a “disorder” is identified, it can then be treated – and for most psychiatrists, this means pills.
Reading his argument, I nodded in agreement – it is important that we (and our children) view negative experiences and the accompanying difficult emotions as part of life’s rich tapestry. That for every up, there will be a down, and often these things are out of our control. Medicating “unfortunate” events not only prevents the individual from fully experiencing, and therefore dealing with, their emotions, but it also gives a false sense of control over our destiny. Shit happens, but we can sort ourselves out with a quick SSRI boost.
But where does PND fall on this spectrum of mental illnesses? Once either considered to be a manifestation of severe baby blues that would sort themselves out in time or women failing to cope with the exigencies of new motherhood, we have a label, a checklist (the Edinburgh scale) and treatment (usually antidepressants and/or some CBT or counselling).
As someone who has benefited from both these treatments, I am grateful for the intervention. After both of my sons were born I was diagnosed with PND and was prescribed Sertaline – and in both instances, my visit to the GP was a lifesaver. I would be furious if someone said my feelings were an inevitable part of having a new baby, and that I’d just have to get over it. So I realise I am being hypocritical in my stance over adding yet more life experiences to DSM -5. Who am I to say that someone grieving the loss of a parent has any less right to access mood-improving medication that I did?
Diana, Princess of Wales, when talking about her bulimia and depression, counselled against the culture of “a pill for every ill” – and urged people to talk more. I think this is where I stand on the issue. I know NHS resources are severely stretched, and that a pack of antidepressants will cost significantly less than a course of CBT. But how about a requirement that GPs who medicate for depressive conditions must also offer counselling or CBT within two months of the appointment?
Yes, I know that sounds expensive – but surely the cost of long-term antidepressant medication and, often, accompanying time off work, is equally, if not more, costly? There are existing recommendations about offering CBT when a patient presents with depressive symptoms, and lip-service paid to antidepressants being a last, rather than a first, resort. But they are not enforced, and waiting times are often so long for counselling (up to a year in some trusts) that people just take the pills and scarper. This can be a great short-term solution (as in my case) but does not help people deal with the behavioural or underlying issues relating to the condition.
I am really pleased that we are acknowledging the reality of mental illness, and that in many areas its stigma is being removed. I certainly feel able to tell people about my PND without shame or embarrassment. But I still want to be able to go through life knowing that sometimes it throws you a curveball, and that it’s ok to feel bad for a while without reaching into the medicine cabinet to make it all better.
Cat Dean blogs at www.postnatalsurvival.com and is author of Fertile Thinking and The Postnatal Survival Guide.






2 Comments
Mat B
February 22, 2013 at 10:35 pm
CBT is a vital and valued psychotherapy (talking therapy) tool that is used in the UK.
It is at present recommended by NICE as first line for mild and moderate depressive illness alone. It is also recommended for the treatment of severe depressive illness with the addition of antidepressants. Whilst there can unfortunately be significant waiting lists, provision of CBT therapy in the UK is good if not universal.
It use in postnatal depression is more limited in part as it often takes longer to have an affect than antidepressants, and in the postnatal period a quick recovery to allow as normal mother and baby life as possible is considered important.
I fundamentally disagree with many of Dr Kinderman’s points about psychiatry at wise, and I do think he fundamentally misrepresents modern psychiatry as practiced in the UK. The major test before any diagnosis is made is that of functional impact. Grief may be normal, but grief that stops you working for months or leaves you unable to even perform basic household chores is not and has a major deleterious effect. The idea that it may not be best dealt with by medicines is definitely nothing new to psychiatric or medical practice but to not call it an “illness” is cruel and perverse undermining the serious effect is has on peoples lives.
Sarah Park
February 24, 2013 at 11:27 pm
Postnatal depression is a challenge every new mom must overcome. It is never easy, but with enough support from families, things will become a lot easier.